This is going to be quick and dirty because I’ve got some other things to do, but I’ve been putting it off far longer than I’ve meant to. (No time like the present, right?) In the January 2008 issue, CR ran a feature on how people could save money on prescriptions meds. Generally speaking, I am in favor of this kind of thing. I like people to know the alternatives, and how they can save money.
Generally-speaking, it’s not a good idea to have word-choice errors in a piece that’s supposed to be professional. (See image.) Maybe they should get a medically-trained copy editor and add them to the list of peer-reviewers. Ridiculous.
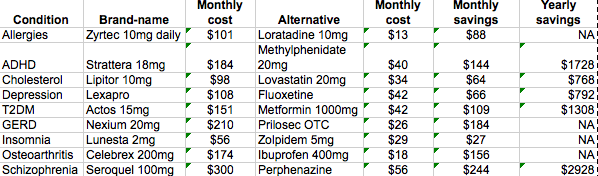
I’ve re-created the table they have:
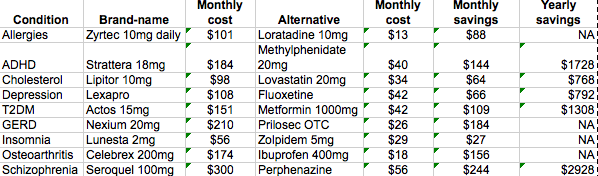
I’ll go through it quickly:
Zyrtec is now available OTC, and is comparable to the cost of Claritin. Claritin doesn’t work for a goodly number of folks, so Zyrtec is a better option. Zyrtec went OTC the month after this was published — and it wasn’t a big secret that it was going to happen.
For ADHD, Strattera is not a popular option. It doesn’t work for many people, and ADHD people have a hard time remembering to take their meds consistently, which makes this option less desirable, particularly where it takes a little while for Strattera to begin working. I’m surprised this drug was listed at all, as it’s rarely a first-line choice for ADHD spectrum disorders. Even comparing atomoxetine (an NRI) to methylphenidate (a stimulant) is a bit… off, and IMO, does the consumer no favors. Strattera is usually used where someone is at risk for drug abuse or has comorbidities like hypertension or anxiety (iatrogenic or otherwise) and so cannot tolerate stimulants.
Depression… don’t have much to say there. Fluoxetine tends to be more stimulating than Lexapro, and there are other subtle differences (half-life, solubility, etc.), but for most people, switching from one to the other is probably not impossible.
As for Diabetes… well. Using a biguanide is usually the first step in treating metabolic syndrome, and then you add other meds on top of that. I’d be skeptical of any doctor who used Actos before using metformin without a given reason. Diabetes treatment tends to go in stepwise fashion like most other chronic illnesses. Removing a TZD from a pre-existing diabetic regimen can be done, but it’s not as simple (or desirable) as this little blurb makes it seem. And a TZD isn’t normally used as monotherapy. Frankly, I think suggesting Glucotrol rather than metformin would have made more therapeutic sense. And in terms of good use of space, I think think they would have been better going after the ARBs and hypertension in general here.
Heartburn and GERD? Nexium 20mg? Who even uses the 20mg strength Nexium? I see it maybe 3 times a year. They should have done 40mg Nexium and suggested 40mg of Prilosec. (Hilarious sidenote: 40mg Prilosec caps (the one without a generic) cost ~$60 more than 40mg Nexium caps.) Generally, though, this one wasn’t too bad.
Insomnia: Eh, probably okay I guess. Insomnia is a poorly-treated condition in this country, and frankly, I’d rather see other methods explored before reaching for the BZRAs at all. But the BZRAs are the easiest, and they keep patients happy. Unfortunately, not enough time is spent diagnosing the underlying causes of insomnia, resulting in a poorly quality of life. There are differences in the polysomnograms of patients on eszopiclone and zolpidem, too, which are not talked about. I’d rather see ramelteon tried before any BZRA, and also see a psychologist about diagnosing an underlying cause for the insomnia in the first place, if a primary care provider cannot take the time (due to financial considerations) to do it themselves. And 5mg of Ambien might help with sleep induction, but the relatively short half-life will do next to nothing for those with sleep maintenance problems.
I’d rather have seen trazodone suggested, since insomnia is usually secondary to some kind of other psychiatric disturbance — a type of uni- or bipolar depression.
Not much to say about arthritis, but I hardly ever see Celebrex used anymore. Now that it stands alone as a COX-2 inhibitor, it’s also the most expensive anti-inflammatory in the book and insurers are loathe to use it. I’d rather see diclofenac recommended over ibuprofen, and suggesting that 400mg of ibuprofen daily is anywhere near equivalent to 200mg of celecoxib is laughable.
Schizophrenia. SCHIZO-FREAKIN-PHRENIA? CR is going to tackle SCHIZOPHRENIA in an article about how to save money?!?! I am having difficulty wrapping my brain around that one.
But okay, here goes. Schizophreniform disorders should be managed by a psychiatrist or psychiatric NP, IMNSHO. Diagnosis is tricky, and management is always tricky. All that said… while first generation antipsychotics are often as effective as their second gen counterparts, I am extremely leery of merely saying that Y could be substituted for X. At least CR has the good grace to state “The antipsychotics have major side effects and response to them is highly variable” — AKA “Take our advice with a monster grain of salt.” Not the least of the worries are akathisia, tardive dyskinesia, other extrapyramidal symptoms, weight gain, and about a bazillion other possible side effects. My mind is still boggled that they even went there.
Curiously, however, discontinuation rates of perphenazine in schizophrenic patients are lower than with any second gen antipsychotic save olanzapine (Zyprexa) — though people tended to d/c Zyprexa due to its metabolic effects and weight gain, and perphenazine for its extrapyramidal symptoms. Something to consider, I suppose.
—
All things considered, it’s nice to see the mainstream media promoting saving money on drugs, but it bugs me that they did it in the way that they did.